Collection rate from insured patients declined by 8.3% last year compared with 2023
Hospitals, health systems and medical practices faced insurance claims practices that slowed payments for needed medical care in 2024 compared with 2023, new Kodiak Solutions revenue cycle data show.
This press release features multimedia. View the full release here: https://www.businesswire.com/news/home/20250521892947/en/
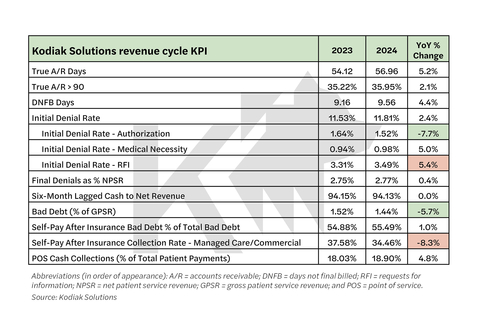
Hospitals, health systems and medical providers faced higher initial claims denials from insurers and a lower collection rate from the self-pay portion of claims for insured patients in 2024 compared with the previous year, according to Kodiak Solutions' proprietary data.
Medical providers also collected about $3 less for every $100 dollars that insured patients owed on their portion of their medical bills, the data also show. The data are from more than 2,100 hospitals and 300,000 physicians that use the Kodiak Revenue Cycle Analytics platform to manage their net revenue and monitor their revenue cycle performance.
The initial denial rate on claims in 2024 increased 2.4% to 11.81% of claims in 2024. The rate climbed even as medical providers have managed to cut the rate of initial denials related to authorization issues by 7.7%. Denials related to questions of medical necessity and requests for more information (RFI) more than made up the difference, with the rates for both categories increasing by 5% and 5.4%, respectively. Kodiak Solutions first highlighted the increase in RFI initial denials in August 2024.
“Payors appear to be using initial denials to slow payments, even though they ultimately pay approximately 90% of claims, a trend we have been tracking,” said Matt Szaflarski, Kodiak’s vice president, revenue cycle intelligence. “Even if the claims are ultimately paid, initial denials still cost hospitals, health systems and medical providers a lot of resources to overturn, and they also slow cash flow.”
Kodiak Solutions data show that true accounts receivable (AR) days increased 5.2% year-over-year.
Provider organizations collected 34.46% of amounts owed by insured patients, down 8.3% from 2023’s self-pay rate for insured patients of 37.58%.
Lessons from revenue cycle leaders
Conversations with leaders of health systems that were recognized in Kodiak’s annual Revenue Cycle Performance Awards yielded tips for improving performance that are detailed in the May 2025 Kodiak RCA Benchmarking Analysis. These high-performing revenue cycle teams shared three attributes:
- A close working relationship with clinical leaders
- Accountability for team members to revenue cycle performance metrics
- Strong relationships with payors.
To learn more about the data and insights Kodiak Solutions can provide to benchmark your revenue cycle performance, contact Szaflarski at (463) 270-8123.
About Kodiak Solutions
Kodiak Solutions is a leading technology and tech-enabled services company that simplifies complex business problems for healthcare provider organizations. For nearly two decades as a part of Crowe LLP, Kodiak created and developed our proprietary net revenue reporting solution, Revenue Cycle Analytics. Kodiak also provides a broad suite of software and services in support of CFOs looking for solutions in financial reporting, reimbursement, revenue cycle, risk and compliance, and unclaimed property. Kodiak’s 450 employees engage with more than 2,100 hospitals and 300,000 practice-based physicians, across all 50 states, and serve as the unclaimed property outsourcing provider of choice for more than 2,000 companies. To learn more, visit our website.
View source version on businesswire.com: https://www.businesswire.com/news/home/20250521892947/en/
“Payors appear to be using initial denials to slow payments, even though they ultimately pay approximately 90% of claims, a trend we have been tracking." -- Matt Szaflarski, Kodiak’s vice president, revenue cycle intelligence
Contacts
For Media:
Vince Galloro
(312) 625-2137
vince.galloro@sunrisehlth.com
